Health equity is achieved when everyone can attain their full potential for health and well-being.
WHO
Contemporary public health and health care face resource constraints, self-regarding versus other-regarding preferences, and strains to become more efficient at less costs, while maintaining quality. Thus, diverse distinct ethical and moral questions and challenges arise. These concerns inevitably imply some involvement of the state that has to intervene through stewardship and governance. In doing so governments seek to promote (aggregate) utility, increase value for money, and foster health equity, while adhering to principles of distributive and procedural justice (Hecht et al. 2019). Globally nations have found a wealth of ways to reach and improve on these objectives. “Moral justifications for public health activities, including overall benefit, collective efficiency, distributive fairness, and harm prevention, are considered by way of examining global human resources for health, with an eye to efficiency, equity, rights, and other ethical issues” (Merritt & Hyder 2019, p. 109). In striving for justice “we must also consider how to distribute whatever is measured. Noncorrelative principles do not try to correlate how much each individual receives with other facts about that individual, whereas correlative principles do” (Persad 2019, p. 36).
Public health aims to mitigate the negative effects of socio-economic determinants of health outcomes, as well as countering health disparities (Venkatapuram 2019). These patterns and gradients, which harm individual, community and public health, are even exacerbated for vulnerable, high-risk and marginalised populations. Such health “stressors may include historic injustices, discrimination and stigmatization, and unique social or physical needs, limitations, or vulnerabilities. […] Included groups are ageing populations, children and adolescents, persons with mental illness, persons with disabilities, sexual and gender minorities, and immigrants and refugees” (Bernheim & Fenton 2019, p. 175).
This project draws four thematic blocks from what has just been laid out:
- It is necessary to investigate the status-quo of vulnerable groups and minorities in terms of (public) health more closely. This then requires research on the effects of socio-economic and health-related characteristics on the health care certain populations receive within a heterogeneous society.
- When comparing the demand side with the supply side of health care patterns of health (in)equities must be made visible.
- Following from the two previous passages, it is imperative to involve considerations of distributive justice in the design of any health policy and of any change in the health care system, especially in areas where resource scarcity and the respective allocation are aggravated, but also in areas of existing inertia.
- Last, there is a need to address the role of the state and of private entities in health care because (public) health care involves several common and public goods. This pertains to what is known as the “public-private mix” in health care, as well as to “one-tiered” versus “two/multiple-tiered health care”.
Aligning these four spheres, I enquire:
What are the effects of asymmetric socio-economic determinants of health and of health disparities on health care access, affordability, and provision?
What does Vienna’s public view as just/fair or unjust/unfair in the city’s public-private health care system in terms of access, affordability, and provision of medical interventions and of health care?
Which health inequities become traceable by comparing population-specific needs with shortfalls in access, affordability, and provision of health care?
Which health policies and resource allocations does Vienna’s public prefer in the city’s public-private health care system?
Theoretical Concept
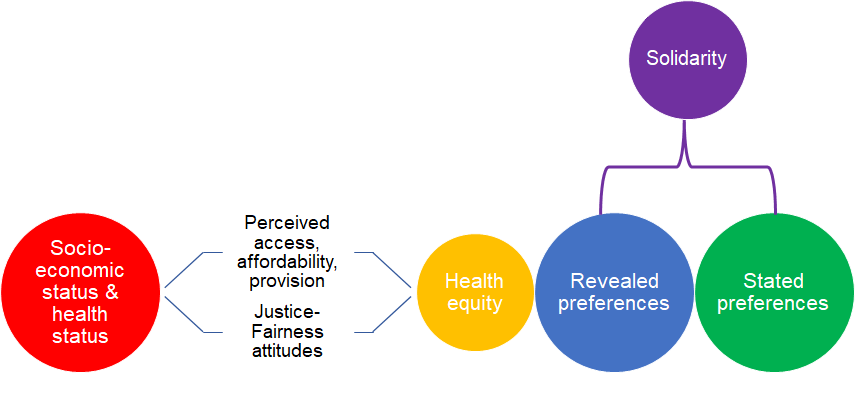
First, the associations between socio-economic and health status with perceived access to, affordability and provision of health care will be elucidated in order to identify health inequities. Second, the comparison between perceptions and attitudes in relation to socio-economic status and health status will allow to derive revealed preferences from. It will be possible to analyse which socio-economic strata, vulnerable and marginalised populations, as well as the public at large, prefer which policies for access, affordability and provision. The successive stated preferences will explicitly consider the “efficiency-equity trade-off”, the balance of the “public-private health care mix” and the tension between “one-and two-tiered health care”. Last, social norms of solidarity, which are expressed as individual practices in human relations, moderate the relationship between socio-economic and individual health, and the sets of preferences. It is ultimately addressing what Peragine (1999, p. 37) called:”(i) the measurement of individuals’ opportunity sets, (ii) the measurement of the degree of inequality present in a distribution of opportunities, and (iii) the design of redistribution mechanisms intended to increase the degree of `opportunity equality'”.
Methods & Data
Concerning data collection the Vienna Public Health Equity Project (ViePHEP) will rely on a one-time survey among the Viennese resident population, with a minimum age of 18 years. The survey sample should be structured as to represent the city’s real resident population, thereby relying on information from the official census.
The ViePHEP survey will gather standard socio-demographic information, e.g. gender, age and education level, of each respondent. Subsequently, the survey will be structured in eight additional modules, each with a set of some questions:
- Health, e.g. self-reported health status, presence of one or several chronic diseases, disorders or disabilities, and behaviours that harm or promote good health
- Socio-economic status in society, e.g. occupation, income, wealth
- Access to health care
- Affordability of health care
- Provision of health care
- Justice-Fairness attitudes
- Preferences for health policies, e.g. design of private vis-à-vis statutory social health insurance, preferred funding of public health budgets, and stated preferences for elements of health care as public, common, club or private goods
- Solidarity as a set of shared social and distributive norms and as a common practice of persons among a social structure with similarities and differences
Targets
Provide Evidence
The first main target of the ViePHEP is to deliver methodologically and empirically robust evidence that can be used as base for further research and for policy making.
Promote Open Science
The ViePHEP strives for a transparent and well documented practice of research to be accessible to both the scientific community and the public.
Improve Health Care
Through the upper targets and by engaging with stakeholders in a Health in All Policies (HiAP) approach the ViePHEP aims at ultimately improving health care.
References
Bernheim, R. G., & Fenton, E. (2019). An Overview of Ethics Issues for Public Health in Particular Populations. In A. C. Mastroianni, J. P. Kahn, & N. E. Kass (Eds.), The Oxford handbook of public health ethics (pp. 173–180). Oxford University Press. https://doi.org/10.1093/oxfordhb/9780190245191.013.15
Hecht, R., Arias, D., & Krubiner, C. (2019). Responsible Resource Allocation, Public Health Stewardship, and Ethics. In A. C. Mastroianni, J. P. Kahn, & N. E. Kass (Eds.), The Oxford handbook of public health ethics (pp. 829–841). Oxford University Press. https://doi.org/10.1093/oxfordhb/9780190245191.013.72
Merritt, M. W., & Hyder, A. A. (2019). An Overview of the Ethics of Health Systems. In A. C. Mastroianni, J. P. Kahn, & N. E. Kass (Eds.), The Oxford handbook of public health ethics (pp. 107–114). Oxford University Press. https://doi.org/10.1093/oxfordhb/9780190245191.013.10
Peragine, V. (1999). The Distribution and Redistribution of Opportunity. Journal of Economic Surveys. Vol. 13, pp. 37-70. https://doi.org/10.1111/1467-6419.00074
Persad, G. (2019). Justice and Public Health. In A. C. Mastroianni, J. P. Kahn, & N. E. Kass (Eds.), The Oxford handbook of public health ethics (pp. 32–46). Oxford University Press. https://doi.org/10.1093/oxfordhb/9780190245191.013.4
Venkatapuram, S. (2019). Health Disparities and the Social Determinants of Health: Ethical and Social Justice Issues. In A. C. Mastroianni, J. P. Kahn, & N. E. Kass (Eds.), The Oxford handbook of public health ethics (pp. 265–276). Oxford University Press. https://doi.org/10.1093/oxfordhb/9780190245191.013.24

